Monoamine releasing agent

A monoamine releasing agent (MRA), or simply monoamine releaser, is a drug that induces the release of one or more monoamine neurotransmitters from the presynaptic neuron into the synapse, leading to an increase in the extracellular concentrations of the neurotransmitters and hence enhanced signaling by those neurotransmitters.[2][3][4][1][5] The monoamine neurotransmitters include serotonin, norepinephrine, and dopamine; MRAs can induce the release of one or more of these neurotransmitters.[2][3][4][1][5]
MRAs work by reversing the direction of the monoamine transporters (MATs), including the serotonin transporter (SERT), norepinephrine transporter (NET), and/or dopamine transporter (DAT), causing them to promote efflux of non-vesicular cytoplasmic monoamine neurotransmitter rather than reuptake of synaptic monoamine neurotransmitter.[5][6][1][7] Many, but not all MRAs, also reverse the direction of the vesicular monoamine transporter 2 (VMAT2), thereby additionally resulting in efflux of vesicular monoamine neurotransmitter into the cytoplasm.[5]
A variety of different classes of drugs induce their effects in the body and/or brain via the release of monoamine neurotransmitters.[2][3] These include psychostimulants and appetite suppressants acting as dopamine and norepinephrine releasers like amphetamine, methamphetamine, and phentermine; sympathomimetic agents acting as norepinephrine releasers like ephedrine and pseudoephedrine; non-stimulant appetite suppressants acting as serotonin releasers like fenfluramine and chlorphentermine; and entactogens acting as releasers of serotonin and/or other monoamines like MDMA.[2][3] Trace amines like phenethylamine and tryptamine, as well as the monoamine neurotransmitters themselves, are endogenous MRAs.[2][3][4] It is thought that monoamine release by endogenous mediators may play some physiological regulatory role.[4]
MRAs must be distinguished from monoamine reuptake inhibitors (MRIs) and monoaminergic activity enhancers (MAEs), which similarly increase synaptic monoamine neurotransmitter levels and enhance monoaminergic signaling but work via distinct mechanisms.[5][1][8][9]
Types and selectivity
[edit]MRAs can be classified by the monoamines they mainly release, although these drugs lie on a spectrum:[2][3][4][5]
- Selective for one neurotransmitter
- Norepinephrine releasing agent (NRA) (e.g., ephedrine, levomethamphetamine)
- Dopamine releasing agent (DRA) (no robustly selective agents known)
- Serotonin releasing agent (SRA) (e.g., chlorphentermine, MMAI)
- Non-selective, releasing two or more neurotransmitters
- Norepinephrine–dopamine releasing agent (NDRA) (e.g., amphetamine, methamphetamine)
- Serotonin–norepinephrine releasing agent (SNRA) (e.g., fenfluramine, MDAI)
- Serotonin–dopamine releasing agent (SDRA) (e.g., 5-chloro-αMT, BK-NM-AMT)
- Serotonin–norepinephrine–dopamine releasing agent (SNDRA) (e.g., MDMA, mephedrone)
The differences in selectivity of MRAs is the result of different affinities as substrates for the monoamine transporters, and thus differing ability to gain access into monoaminergic neurons and induce monoamine neurotransmitter release.
As of present, no selective DRAs are known. This is because it has proven extremely difficult to separate DAT affinity from NET affinity and retain releasing efficacy at the same time.[10] Several selective SDRAs, including tryptamine, (+)-α-ethyltryptamine (αET), 5-chloro-αMT, and 5-fluoro-αET, are known.[11][12] However, besides their serotonin release, many of these compounds additionally act as non-selective serotonin receptor agonists, including of the serotonin 5-HT2A receptor (with accompanying hallucinogenic effects), and some of them are known to act as monoamine oxidase inhibitors.[11][12]
Effects and uses
[edit]MRAs can produce varying effects depending on their selectivity for inducing the release of different monoamine neurotransmitters.[3]
Selective SRAs such as chlorphentermine have been described as dysphoric and lethargic.[13][14] Less selective SRAs that also stimulate the release of dopamine, such as methylenedioxymethamphetamine (MDMA), are described as more pleasant, more reliably elevating mood and increasing energy and sociability.[15] SRAs have been used as appetite suppressants and as entactogens. They have also been proposed for use as more effective antidepressants and anxiolytics than selective serotonin reuptake inhibitors (SSRIs) because they can produce much larger increases in serotonin levels in comparison.[16]
DRAs, usually non-selective for both norepinephrine and dopamine, have psychostimulant effects, causing an increase in energy, motivation, elevated mood, and euphoria.[17] Other variables can significantly affect the subjective effects, such as infusion rate (increasing positive effects of DRAs) and psychological expectancy effects.[18] They are used in the treatment of attention deficit hyperactivity disorder (ADHD), as appetite suppressants, wakefulness-promoting agents, to improve motivation, and are drugs of recreational use and misuse.
Selective NRAs are minimally psychoactive, but as demonstrated by ephedrine, may be distinguished from placebo, and may trends towards liking.[19] They may also be performance-enhancing,[20] in contrast to reboxetine which is solely a norepinephrine reuptake inhibitor.[21][22] In addition to their central effects, NRAs produce peripheral sympathomimetic effects like increased heart rate, blood pressure, and force of heart contractions. They are used as nasal decongestants and bronchodilators, but have also seen use as wakefulness-promoting agents, appetite suppressants, and antihypotensive agents. They have additionally seen use as performance-enhancing drugs, for instance in sports.
Mechanism of action
[edit]Mechanisms of monoamine release by MRAs
[edit]MRAs induce the release of the monoamine neurotransmitters serotonin, norepinephrine, and/or dopamine from monoaminergic neurons in the brain and/or periphery.[3][23][24] MRAs are substrates of the plasma membrane-associated monoamine transporters (MATs), including of the serotonin transporter (SERT), norepinephrine transporter (NET), and/or dopamine transporter (DAT), and enter presynaptic monoaminergic neurons via these transporters.[23][3][24][25] To a much lesser extent, sufficiently lipophilic MRAs may also passively diffuse into monoaminergic neurons.[23][24] Once in the intracellular space of the neuron, MRAs reverse the direction of the MATs, as well as of the organic cation transporter 3 (OCT3),[23][26] such that they mediate efflux of cytosolic monoamine neurotransmitters into the extracellular synaptic cleft rather than the usual reuptake.[23][24] Many, though notably not all MRAs,[5][27][note 1] additionally act at the vesicular monoamine transporter 2 (VMAT2) on synaptic vesicles to enhance the pool of cytosolic monoamine neurotransmitters available for efflux.[23][5][31][24] However, MRAs can still induce monoamine release without VMAT2, for instance by releasing newly synthesized cytosolic neurotransmitters.[23][32][33] In addition to their induction of monoamine release, MRAs act less potently as monoamine reuptake inhibitors (MRIs).[23][24][2][1] This is due to substrate competition with monoamine neurotransmitters for the MATs[25][6][1] and/or induction of MAT internalization and consequent inactivation.[23][34] The monoamine neurotransmitters released by MRAs bind to and activate monoamine receptors on presynaptic and postsynaptic neurons to facilitate monoaminergic neurotransmission.[25][35] As such, MRAs can be described as indirect monoamine receptor agonists.[35][1]
The mechanisms by which MRAs induce MAT reverse transport and efflux are complex and incompletely understood.[23][24][36][37] The process appears to depend on a number of intracellular changes, including sodium ion (Na+) and calcium ion (Ca2+) elevation, protein kinase C (PKC) activation, and Ca2+/calmodulin-dependent protein kinase II alpha (CaMKIIα) activation, among others.[24][23][36][37][38] Activation of protein kinases including PKC, CaMKIIα, and others results in phosphorylation of the MATs causing them to mediate efflux instead of reuptake.[23][36][39][34] Exactly how MRAs induce the preceding effects is unclear however.[23][24][36][34][37] A more recent study suggests that intracellular Ca2+ elevation, PKC activation, and CaMKIIα might all be dispensable for MRA-induced monoamine release, but more research is needed.[40]
The trace amine-associated receptor 1 (TAAR1) is a receptor for trace amines like β-phenethylamine and tryptamine, as well as for monoamine neurotransmitters like dopamine and serotonin, and is a known target of many MRAs, such as amphetamine and methamphetamine.[41] The TAAR1 is a largely intracellular receptor expressed both in presynaptic and postsynaptic monoaminergic neurons and appears to be extensively co-localized with MATs in the brain.[42][41] Some in-vitro studies have found that TAAR1 agonism by MAT substrates like MRAs can produce PKC activation and thereby induce MAT reverse transport and monoamine efflux.[42][43] As such, TAAR1 agonism, coupled with MAT substrate activity, could mediate or contribute to the monoamine release of MRAs.[42][43] However, findings in this area are conflicting, with other studies unable to replicate the results.[44][45][46][47][48][49] In addition, MRAs can still induce monoamine efflux in the absence of TAAR1 in vitro,[50][51][42] well-known MRAs like amphetamine and methamphetamine exhibit only low-potency human TAAR1 agonism[52][53][35] that is of uncertain general significance in humans,[26][54][55][56][57] many other MRAs are inactive as TAAR1 agonists in humans,[52][53][25][26][note 2] the monoamine release and behavioral effects of amphetamines are not only preserved but substantially augmented in TAAR1 knockout mice,[44][42] and the monoamine release and behavioral effects of amphetamines are strongly reduced or abolished in mice with TAAR1 overexpression.[44][59] Besides induction of monoamine release, TAAR1 agonism, as well as other mechanisms, may mediate MAT internalization.[23][60] MAT internalization may limit the capacity of MRAs to induce MAT reverse transport and monoamine efflux.[61][62] TAAR1 signaling also activates G protein-coupled inwardly rectifying potassium channels (GIRKs) and thereby robustly inhibits the firing rates of brain monoaminergic neurons and suppresses exocytotic monoamine release.[63][42][46] Due to the preceding mechanisms, potent TAAR1 agonism by MRAs that possess this action may actually auto-inhibit and constrain their monoaminergic effects.[56][26][64][49]
Although induction of MAT reverse transport and consequent monoamine efflux is the leading theory of how MRAs act, an alternative and more recent theory has proposed that amphetamine, at therapeutic doses, may not actually act by inducing DAT reverse transport and dopamine efflux, but instead by augmenting exocytotic dopamine release and hence by enhancing phasic rather than tonic dopaminergic signaling.[23][65][66] According to this model, DAT reverse transport may only be relevant at supratherapeutic doses and may be more associated with toxicity, for instance induction of psychosis.[23][65][66] It is unclear how amphetamine might act to enhance exocytotic dopamine release, and more research is needed to evaluate this theory.[23][65][66]
Aside from the mechanisms mediating the monoamine release of MRAs, other targets of some MRAs, such as the intracellular sigma σ1 receptor, have been found to inhibit MRA-induced monoamine efflux via interactions with the MATs.[67][68] Conversely, activation of the sigma σ2 receptor has been found to potentiate amphetamine-induced dopamine efflux.[69] The mechanism mediating this effect is unknown, but it has been postulated that it may be due to elevation of intracellular calcium and consequent downstream effects.[69]
Differences from physiological release and reuptake inhibitors
[edit]The neurotransmitter release induced by MRAs is very different from normal exocytotic monoamine release, in which action potentials trigger synaptic vesicles to fuse with the cell membrane and release neurotransmitters into the synaptic cleft.[23][3] In relation to this, MRAs promote tonic monoaminergic signaling, whereas normal exocytotic monoamine release involves phasic monoaminergic signaling.[23]
The enhancement of monoaminergic signaling by MRAs also differs from that with MRIs.[3][5][23][36] Because MRIs block monoamine neurotransmitter reuptake and consequent inactivation following action potentials and exocytotic release, they preferentially augment phasic monoaminergic signaling rather than tonic signaling.[3] In addition, inhibitory presynaptic and somatodendritic monoamine autoreceptors, including serotonin 5-HT1A and 5-HT1B autoreceptors, dopamine D2 and D3 autoreceptors, and α2-adrenergic autoreceptors, respond to elevated synaptic monoamine neurotransmitter levels by inhibiting presynaptic monoaminergic neuron firing rates, and this substantially limits the effects of MRIs.[3][5][35] In contrast, MRAs do not depend on action potentials to induce monoamine release, and thus are able to largely bypass the negative feedback mediated by autoreceptors.[3] Relatedly, MRAs can induce far greater maximal increases in monoamine neurotransmitter levels than MRIs.[3] For instance, MRIs can achieve maximal elevations in brain monoamine levels of about 5- to 10-fold in animals, whereas MRAs can produce elevations of as much as 10- to 50-fold, with no clear ceiling limit.[1][70][71][72][73][3][74] Since MRAs depend on uptake by the MATs to induce monoamine release, their mediation of monoamine release and consequent effects can be blocked by MRIs.[3][23][24][75]
Structural requirements and partial MRAs
[edit]
There is a constrained and relatively small molecular size requirement for compounds to act as MRAs.[5] This is because they must be small enough to serve as substrates of the monoamine transporters and thereby be transported inside of monoaminergic neurons by these proteins, in turn allowing them to induce monoamine neurotransmitter release.[5][23] Compounds with chemical features extending beyond the size constraints for releasers will instead act as partial releasers, reuptake inhibitors, or be inactive.[5][23] Partial releasers show reduced maximal efficacy in releasing monoamine neurotransmitters compared to conventional full releasers.[5][6][23] While most MRAs are full releasers, a number of partial releasers are known and may have atypical properties.[5][6] Examples of partial releasers include 3,4-methylenedioxyethylamphetamine (MDEA), N-ethylnaphthylaminopropane (ENAP), 3-trifluoromethyl-4-chlorophenylpiperazine (TFMCPP), para-nitrophenylpiperazine (pNPP), bretisilocin, and psilocin.[5][6][76][77][78] The mechanisms responsible for the differences between full releasers and partial releasers are largely unknown.[6]
Other related agents
[edit]DAT "inverse agonists"
[edit]Dopamine reuptake inhibitors (DRIs) have been grouped into two types, typical or conventional DRIs like cocaine, WIN-35428 (β-CFT), and methylphenidate that produce potent psychostimulant, euphoric, and reinforcing effects, and atypical DRIs like vanoxerine (GBR-12909), modafinil, benztropine, and bupropion, which do not produce such effects or have greatly reduced such effects.[7][6][5][79] It has been proposed that typical DRIs may not actually be acting primarily as DRIs but rather as dopamine releasing agents (DRAs) via mechanisms distinct from conventional substrate-type DRAs like amphetamines.[7] A variety of different pieces of evidence support this hypothesis and help to explain otherwise confusing findings.[7] For example, typical DRIs like cocaine and methylphenidate can robustly increase brain dopamine levels similarly to substrate-type DRAs like amphetamine, whereas atypical DRIs, which are viewed as simple competitive reuptake inhibitors, achieve much more modest increases.[7][80][81][82] Under this model, typical cocaine-like DRIs have been referred to with the new label of dopamine transporter (DAT) "inverse agonists" to distinguish them from conventional substrate-type DRAs.[7] An alternative theory is that typical DRIs and atypical DRIs stabilize the DAT in different conformations, with typical DRIs resulting in an outward-facing open conformation that produces differing pharmacological effects from those of atypical DRIs.[6][5][79][83]
Monoaminergic activity enhancers
[edit]Some MRAs, like the amphetamines amphetamine and methamphetamine, as well as trace amines like phenethylamine, tryptamine, and tyramine, are additionally monoaminergic activity enhancers (MAEs).[8][9][84] That is, they enhance the action potential-mediated release of monoamine neurotransmitters (in contrast to MRAs, which induce uncontrolled monoamine release independent of neuronal firing).[8][9][84] They are usually active as MAEs at much lower concentrations than those at which they induce monoamine release.[8][9][84] The MAE actions of MAEs may be mediated by TAAR1 agonism, which has likewise been implicated in monoamine-releasing actions in some studies.[85][86][87] MAEs without concomitant potent monoamine-releasing actions, like selegiline (L-deprenyl), phenylpropylaminopentane (PPAP), and benzofuranylpropylaminopentane (BPAP), have been developed.[8][9]
Endogenous MRAs
[edit]A number of endogenous compounds are known to act as MRAs.[4][88][77][11][5] These include the monoamine neurotransmitters dopamine (an NDRA),[88] norepinephrine (an NDRA),[88] and serotonin (an SRA) themselves,[88] as well as the trace amines phenethylamine (an NDRA),[5][84][89][90] tryptamine (an SDRA or imbalanced SNDRA),[77][11] and tyramine (an NDRA).[88][4] Synthetic MRAs are substantially based on structural modification of these endogenous compounds, most prominently including the substituted phenethylamines and substituted tryptamines.[88][2][3][77][91][92][93]
Release of monoamine neurotransmitters by themselves, for instance in the cases of serotonin, norepinephrine, and dopamine, has been referred to as "self-release".[4] The physiological significance of the findings that monoamine neurotransmitters can act as releasing agents of themselves is unclear.[4] However, it could imply that efflux is a common neurotransmitter regulatory mechanism that can be induced by any transporter substrate.[4]
It is possible that monoamine neurotransmitter self-release could be a protective mechanism.[4][94] It is notable in this regard that intracellular non-vesicular or cytoplasmic dopamine is toxic to neurons and that the vesicular monoamine transporter 2 (VMAT2) is neuroprotective by packaging this dopamine into synaptic vesicles.[95][96][97][94] Along similar lines, MRAs induce the efflux of non-vesicular monoamine neurotransmitter and thereby move cytoplasmic neurotransmitter into the extracellular space.[5] On the other hand, many MRAs but not all also act as VMAT2 inhibitors and reversers, and hence concomitantly induce the release of vesicular monoamine neurotransmitters like dopamine into the cytoplasm.[5] Induction of VMAT2 efflux by MRAs appears to be related to their monoaminergic neurotoxicity.[35][98][29]
Monoaminergic neurotoxicity
[edit]Some MRAs have been found to act as monoaminergic neurotoxins and hence to produce long-lasting damage to monoaminergic neurons.[99][100] Examples include dopaminergic neurotoxicity with amphetamine and methamphetamine and serotonergic neurotoxicity with methylenedioxymethamphetamine (MDMA).[99][100] Amphetamine may produce significant dopaminergic neurotoxicity even at therapeutic doses.[101][102][103][104][105][106] However, clinical doses of amphetamine producing neurotoxicity is controversial and disputed.[107][101][103] In contrast to amphetamines, monoamine reuptake inhibitors like methylphenidate lack apparent neurotoxic effects.[101]
Analogues of MDMA with retained MRA activity but reduced or no serotonergic neurotoxicity, like 5,6-methylenedioxy-2-aminoindane (MDAI) and 5-iodo-2-aminoindane (5-IAI), have been developed.[28][108] Certain drugs have been found to block the neurotoxicity of MRAs in animals.[100] For instance, the selective MAO-B inhibitor selegiline has been found to prevent the serotonergic neurotoxicity of MDMA in rodents.[100]
Chemical families
[edit]MRAs are usually arylalkylamines. A number of different structural families of compounds have been found to act as MRAs. The possible structural forms of MRAs are limited by a small molecular size requirement for activity.[5] Molecules that are too large become monoamine reuptake inhibitors as they can no longer be transported into neurons by the monoamine transporters and induce monoamine release intracellularly.[5]
Phenethylamine-like
[edit]- Phenethylamines (2-phenylethylamines) (e.g., phenethylamine, tyramine, dopamine, norepinephrine)
- Amphetamines (α-methylphenethylamines) (e.g., amphetamine, methamphetamine, fenfluramine)
- Cathinols (β-hydroxyamphetamines) (e.g., phenylpropanolamine, ephedrine, pseudoephedrine, cathine)
- Cathinones (β-ketoamphetamines) (e.g., cathinone, methcathinone, mephedrone)
- Phentermines (α-methylamphetamines) (e.g., phentermine, mephentermine, chlorphentermine, clortermine)
- Phenylisobutylamines (α-ethylphenethylamines) (e.g., phenylisobutylamine, 4-CAB, 4-MAB, buphedrone)
- Ring-extended amphetamines
- Benzodioxolylaminopropanes (methylenedioxyamphetamines) (e.g., MDA, MDMA, MDEA, methylone)
- Methylenedioxycathinones (e.g., methylone, ethylone, butylone)
- Methylenedioxyphentermines (e.g., MDPH, MDMPH)
- Benzodioxolylisobutylamines (e.g., BDB, MBDB, butylone)[109]
- Benzodioxanylaminopropanes (ethylenedioxyamphetamines) (e.g., EDA, EDMA, EDMC)[110][111][112]
- Benzofuranylaminopropanes (e.g., 4-APB, 5-APB, 5-MAPB, 6-APB, 6-MAPB, 5-APDB, 5-MAPDB, 6-APDB, 6-MAPDB, 7-APB, IBF5MAP)[113][114][115]
- Benzofuranylisobutylamines (e.g., 5-MBPB, 6-MBPB)[116]
- Benzothiophenylaminopropanes (e.g., 4-APBT, 5-APBT, 5-MAPBT, 6-APBT, 7-APBT)[117]
- Indolylaminopropanes (e.g., 5-IT/5-API, 6-IT/6-API)[118]
- Indanylaminopropanes (e.g., 5-APDI/IAP, 5-MAPDI)[115][119]
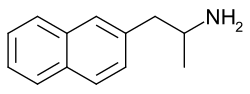
- Naphthylaminopropanes (e.g., NAP, methamnetamine/MNAP, ENAP, BMAPN)[76][120]
- Tetralinylaminopropanes (e.g., 6-APT/TAP)[115]
- Other ring-extended amphetamines (e.g., ODMA,[121] SeDMA,[121] TDMA[121])
- Benzodioxolylaminopropanes (methylenedioxyamphetamines) (e.g., MDA, MDMA, MDEA, methylone)
- Amphetamines (α-methylphenethylamines) (e.g., amphetamine, methamphetamine, fenfluramine)
- Cyclopentylaminopropanes (e.g., isocyclamine, cyclopentamine)[122]
- Cyclohexylaminopropanes (e.g., norpropylhexedrine, propylhexedrine)[122]
- Phenylpropylamines (e.g., phenylpropylamine, homo-MDA, homo-MDMA)[123][4][124][125]
- Thiophenylisopropylamines (e.g., thiopropamine, methiopropamine, thiothinone)[126]
- Phenylalkenylamines and phenylalkynylamines (e.g., phenylbutynamine, phenylbutenamine)[127][128][76]
- Other possible groups (e.g., 2-furylethylamines, 2-tetrahydrofurylethylamines, 2-pyrrolylethylamines, 3-pyrrolylethylamines)[93][126]
Amine fused into ring
[edit]- Phenylalkylpyrrolidines (e.g., α-PPP, 4-MePPP)[129][130]
- Phenylmorpholines (e.g., phenmetrazine, phendimetrazine)
- Phenyloxazolamines (e.g., aminorex, 4-methylaminorex, pemoline)
- Benzylpiperazines (e.g., 1-benzylpiperazine, MBZP)
- Methylenedioxybenzylpiperazines (e.g., MDBZP, fipexide)
- Benzylpiperidines (e.g., 4-benzylpiperidine)
- Phenylpiperazines (e.g., 1-phenylpiperazine, mCPP, TFMPP, oMPP, pFPP, pMeOPP)[131]
Alkyl chain fused into ring
[edit]- 2-Aminoindanes (e.g., 2-aminoindane (2-AI), NM-2-AI, MMAI, MEAI, ETAI, TAI, 5-IAI)[33][132][120]
- Methylenedioxyaminoindanes (e.g., MDAI, MDMAI)[33][132]
- Benzofurancyclopentanylamines (e.g., BFAI)[133]
- 2-Aminotetralins (e.g., 2-aminotetralin, 6-CAT)[132][120]
- Methylenedioxyaminotetralins (e.g., MDAT, MDMAT)[132]
- Other possible groups (e.g., benzylamines (e.g., MDM1EA),[125] 2-amino-1,2-dihydronaphthalenes (e.g., 2-ADN),[134][135] aminobenzocycloheptenes (e.g., 6-AB, 7-AB)[120][136])
Tryptamine-like
[edit]- Tryptamines (2-(3-indolyl)ethylamines) (e.g., tryptamine, serotonin, bufotenin, DMT, psilocin, bretisilocin)[77][11]
- α-Alkyltryptamines (e.g., αMT (3-API), αET, 5-chloro-αMT, 5-fluoro-αMT)[11][109]
- Isotryptamines (2-(1-indolyl)ethylamines) (e.g., isoAMT)[12]
- Indolizinylaminopropanes (e.g., 1ZP2MA, 1Z2MAP1O)[139][140]
- Benzothiophenylaminopropanes (e.g., 2-APBT, 3-APBT)[117]
- Benzofuranylaminopropanes (e.g., 2-APB, 2-MAPB, 3-APB)[114]
- Other possible groups (e.g., 2-pyrrolylethylamines, 3-pyrrolylethylamines)[93][126]
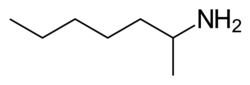
Ring-less (alkylamines)
[edit]- Alkylamines (e.g., 1,3-DMBA,[60] 1,4-DMAA,[60][141] heptaminol,[142][143] iproheptine, isometheptene,[142] methylhexanamine/1,3-DMAA,[60][35][141][144] octodrine,[60][145] oenethyl,[146][147] tuaminoheptane[60][142][148][143])[146][122]
Chemical family structures gallery
[edit]Activity profiles
[edit]The activities of many MRAs in terms of their potencies, efficacies, and selectivities for monoamine release induction in vitro have been characterized in numerous studies in the scientific literature.[2][71][3][5][149] These studies have been especially conducted by the research lab led by Richard B. Rothman and Michael H. Baumann at the National Institute on Drug Abuse (NIDA).[2][71][3][149] These researchers developed an assay measuring monoamine release from rat brain synaptosomes in 1999 that has subsequently been widely employed.[149][71][88][150][151] The data with this procedure from many relevant studies are provided in the table below.[2][3] The Rothman and Baumann lab refers to these data as the "Phenyl Amine Library", "Phenethylamine Library", "Phenylethylamine Library", or "PAL" library, a large library of values of phenethylamine analogs at the monoamine transporters (1,400 compounds as of 2015), and has designated PAL-# code names for the drugs included in it.[152][5][149]
Another method of measuring monoamine release involves the use of human HEK293 cells transfected with and expressing monoamine transporters.[51][58][28][153][110] However, MRAs show differing and much lower potencies in this system compared to rat brain synaptosomes, and it is much less frequently employed.[51][58][28][153][110] The reasons for these differences are not entirely clear, but may be related to species differences, differences in release assay methods, and/or absence of important neuronal membrane proteins in non-neuronal HEK293 cells.[110][50]
| Compound | PAL # | 5-HT | NE | DA | Type | Class | Ref |
|---|---|---|---|---|---|---|---|
| 1-Methyl-T | PAL-637 | 53.1 | >10000 | >10000 | SRA | Tryptamine | [11] |
| 1-Phenylpiperazine (PP) | ND | 880 | 186 | 2530 | SNRA | Phenylpiperazine | [131] |
| 1ZP2MA | ND | ND | ND | 61.9 | ND | Indolizinylethylamine | [139] |
| 2-Aminoindane (2-AI, AI) | ND | >10000 | 86 | 439 | NDRA | Aminoindane | [33] |
| 2-APBT | ND | 8.9 | 21.6 | 38.6 | SNDRA | APBT | [117] |
| 2-BMC | ND | 2837 | 156 | 650 | NDRA | Cathinone | [154] |
| 2-CA | ND | ND | 19.1 | 62.4 | ND | Amphetamine | [4] |
| 2-CMC | ND | 2815 | 93 | 179 | NDRA | Cathinone | [154] |
| 2-FA | ND | ND | 24.1 | 38.1 | ND | Amphetamine | [4] |
| 2-FMA | ND | ~15000 | <100 | ~90 | NDRA | Amphetamine | [citation needed] |
| 2-FMC | ND | >10000 | ND (85% at 10 μM) | 48.7 | NDRA | Cathinone | [137] |
| 2-FPM | ND | 4808 | 28 | 112 | NDRA | Phenylmorpholine | [155] |
| 2-MA | ND | ND | 37 | 127 | ND | Amphetamine | [4] |
| 2-MeO-A | ND | ND | 473 | 1478 | ND | Amphetamine | [4] |
| 2-MeO-MC | ND | 7220 | 339 | 920 | NDRA | Cathinone | [154] |
| 2-MMC | ND | 347–490 | 53 | 81–97.9 | SNDRA | Cathinone | [137][154] |
| 2-MPM | ND | 1758 | 102 | 374 | NDRA | Phenylmorpholine | [156] |
| 2-Phenylmorpholine | PAL-632 | 20260 (31% at 10 μM) | 79 (96% at 10 μM) | 86 (98% at 10 μM) | NDRA | Phenylmorpholine | [157] |
| 2-TFMeO-MC | ND | >10000 | ND (33% at 10 μM) | >10000 | IA | Cathinone | [137] |
| 2-TFMMC (2-TFMAP) | ND | 8400–>10000 | 2200 (69% at 10 μM) | 8000–>10000 | SNDRA | Cathinone | [158][137][159][154] |
| 2C-C | ND | >100000 | >100000 | 100000 | IA | Phenethylamine | [109][160] |
| 2C-D | ND | IA | IA | IA | IA | Phenethylamine | [160] |
| 2C-E | ND | >100000 | >100000 | >100000 | IA | Phenethylamine | [109][160] |
| 2C-I | ND | >100000 | >100000 | >100000 | IA | Phenethylamine | [109][160] |
| 2C-T-2 | ND | IA | IA | IA | IA | Phenethylamine | [160] |
| 3-APBT | ND | 21.9 | 13.4 | 21.7 | SNDRA | APBT | [117] |
| 3-BCPC | PAL-586 | 621 | ND | IA (RI) | ND | Cathinone | [152] |
| 3-BMC | ND | 136–137 | 25 | 21–28.0 | SNDRA | Cathinone | [137][161][154] |
| 3-CA | PAL-304 | 120 | 9.4 | 11.8 | SNDRA | Amphetamine | [123][4][152][162] |
| 3-CC | ND | 567 | 105 | 64 | SNDRA | Cathinone | [163][161] |
| 3-CCPC (RTI-6037-39) | PAL-433 | 1328 | ND | IA (RI) | ND | Cathinone | [152][164] |
| (–)-3-CCPC | PAL-1122 | 562 | ND | IA (RI) | ND | Cathinone | [152] |
| (+)-3-CCPC | PAL-1123 | 733 | ND | IA (RI) | ND | Cathinone | [152] |
| 3-CEC | PAL-361 | IA | ND | IA | ND | Cathinone | [152] |
| 3-Cl-4-Me-CPC | PAL-820 | 181 | ND | IA (RI) | ND | Cathinone | [152] |
| 3′-Cl-5-Me-PM | PAL-738 | 23 (Emax = 96%) | 65 (Emax = 89%) | 58 (Emax = 78%) | SNDRA | Phenylmorpholine | [76][165] |
| 3-CMC (clophedrone) | PAL-434 | 211–410 | 19–54.4 | 26–46.8 | SNDRA | Cathinone | [5][137][161][154][152][166] |
| 3-CPC | PAL-363 | IA | ND | IA (RI) | ND | Cathinone | [152] |
| 3′-CPM | PAL-594 | 301 | 75 (82% at 10 μM) | 27 (100% at 10 μM) | ND | Phenylmorpholine | [165][157] |
| 3-FA | PAL-353 | 1937 | 16.1 | 24.2 | NDRA | Amphetamine | [167][4] |
| 3-FMC | ND | 1460 | ND (100% at 10 μM) | 64.8 | NDRA | Cathinone | [137] |
| 3′-FPM | PAL-593 | 1269–2558 | 17–30 | 43–60 | NDRA | Phenylmorpholine | [155][157] |
| 3-MA | PAL-314 | 218 | 18.3 | 33.3 | NDRA | Amphetamine | [167][123][4] |
| 3-MCPC | PAL-588 | 1067 | ND | IA (RI) | ND | Cathinone | [152] |
| 3-MeO-A | ND | ND | 58.0 | 103 | ND | Amphetamine | [4] |
| 3-MeO-CPC | PAL-591 | 1014 | ND | IA (RI) | ND | Cathinone | [152] |
| 3-MeO-MC | ND | 306–683 | 111 (68% at 10 μM) | 109–129 | SNDRA | Cathinone | [137][161][154] |
| 3-MeO-PM | PAL-823 | ND (78% at 10 μM) | ND (86% at 10 μM) | ND (96% at 10 μM) | ND | Phenylmorpholine | [157] |
| 3-MMC | ND | 268–292 | 27 | 28–70.6 | SNDRA | Cathinone | [5][137][161][154] |
| 3-MPM | PAL-773 | 86 | 62 | 227 | SNDRA | Phenylmorpholine | [156] |
| 3-TFMeO-MC | ND | 188 | ND (79% at 10 μM) | 729 | SNDRA | Cathinone | [137] |
| 3-TFMMC (3-TFMAP) | ND | 297–380 | 2700 (78% at 10 μM) | 610–1290 | SNDRA | Cathinone | [158][137][159][154] |
| 3,4-DCCPC | PAL-787 | 356 | ND | IA (RI) | ND | Cathinone | [152] |
| 4-APBT | ND | 21.2 | 46.2 | 66.6 | SNDRA | APBT | [117] |
| 4-Benzylpiperidine | ND | 5246 | 41.4 | 109 | NDRA | Benzylpiperidine | [168] |
| 4-BMC (brephedrone) | ND | 42.5–60.2 | 100 | 59.4 | SNDRA | Cathinone | [169][137][161][154][170][171] |
| 4-CA (PCA) | ND | 28.3 | 23.5–26.2 | 42.2–68.5 | SNDRA | Amphetamine | [123][4][172][173] |
| 4-CC | ND | 128.4 | 85.1 | 221.8 | SNDRA | Cathinone | [172] |
| 4-CCPC | PAL-743 | 1632 | ND | IA (RI) | ND | Cathinone | [152] |
| 4-CEA (PCEA) | ND | 33.8 | 162.6 | 238.0 | SNDRA | Amphetamine | [172][173] |
| 4-CEC | ND | 152.6 | 5194.0 | 353.6 | SDRA | Cathinone | [172] |
| 4-CMA (PCMA) | ND | 29.9 | 36.5 | 54.7 | SNDRA | Amphetamine | [172][173] |
| 4-CMC (clephedrone) | ND | 71.1–144 | 44–90.9 | 42.2–74.7 | SNDRA | Cathinone | [169][137][172][161][154][170][171] |
| 4-Et-PEA | PAL-505 | ND | ND | 2087 | ND | Phenethylamine | [5] |
| 4-FA | PAL-303 | 730–939 | 28.0–37 | 51.5–200 | NDRA | Amphetamine | [167][109][123][4] |
| 4-Fluoro-T | PAL-551 | 108 | 1123 | 106 | SDRA | Tryptamine | [11] |
| 4-FMC (flephedrone) | ND | 1290–1450 | 62 | 83.4–119 | NDRA | Cathinone | [169][137][161][170][171] |
| 4-FPM | PAL-635 | 2403 (88% at 10 μM) | 285 (100% at 10 μM) | 529 (95% at 10 μM) | SNDRA | Phenylmorpholine | [157] |
| 4′-FPM | PAL-748 | 1895 | 58 | 191 | NDRA | Phenylmorpholine | [155][157] |
| 4-iPr-PEA | PAL-595 | ND | ND | IA | ND | Phenethylamine | [5] |
| 4-MA | PAL-313 | 53.4 | 22.2 | 44.1 | SNDRA | Amphetamine | [167][123][4] |
| 4-MAR | ND | ND | ND | ND | ND | Phenyloxazolamine | [153] |
| cis-4-MAR | ND | 53.2 | 4.8 | 1.7 | NDRA | Phenyloxazolamine | [153][174] |
| 4-MBA | ND | IA | IA | IA | IA | Amphetamine | [175] |
| 4-MCPC | PAL-744 | 667 | ND | IA (RI) | ND | Cathinone | [152] |
| 4-MEA | ND | 102 | 182 | 550 | SNDRA | Amphetamine | [175] |
| 4-MeO-MC (methedrone) | ND | 120–195 | 111 | 506–881 | SNDRA | Cathinone | [169][137][161][154][171] |
| 4-MeO-T | PAL-548 | 4114 | >10000 | >10000 | SRA | Tryptamine | [11] |
| 4-MMA | ND | 67.4 | 66.9 | 41.3 | SNDRA | Amphetamine | [175][170] |
| 4-MPA | ND | 650 | 752 | IA | SNRA | Amphetamine | [175] |
| 4-MPEA (4-Me-PEA) | PAL-503 | ND | ND | 271 | ND | Phenethylamine | [5] |
| 4-MPM | PAL-747 | 86 | 62 | 227 | SNDRA | Phenylmorpholine | [156][157] |
| 4-MTA | ND | ND | ND | ND | ND | Amphetamine | [176][177][178] |
| 4-MTMA | PAL-1063 | 21 | ND | ND | ND | Amphetamine | [76] |
| 4-tBu-MC | ND | IA | ND | 942 (Emax ≈ 50%) | ND | Cathinone | [179] |
| 4-TFMeO-MC | ND | 118 | ND | 7510 | ND | Cathinone | [137] |
| 4-TFMMC (4-TFMAP) | ND | 190–270 | 900 | 2700–4230 | SNRA | Cathinone | [180][169][158][159][171][154] |
| 4,4'-DMAR | ND | ND | ND | ND | SNDRA | Phenyloxazolamine | ND |
| cis-4,4'-DMAR | ND | 17.7–59.9 | 11.8–31.6 | 8.6–24.4 | SNDRA | Phenyloxazolamine | [174][181][153] |
| trans-4,4'-DMAR | ND | 59.9 | 31.6 | 24.4 | SNDRA | Phenyloxazolamine | [181][153] |
| 5-APB | ND | 19 | 21 | 31 | SNDRA | Amphetamine | [113] |
| 5-APBT | ND | 10.3 | 38.4 | 92.8 | SNDRA | APBT | [117] |
| 5-API (5-IT) | PAL-571 | 28–104.8 | 13.3–79 | 12.9–173 | SNDRA | Amphetamine | [12][118] |
| 5-Bromo-T | PAL-518 | 75.0 | >10000 | 478 | SDRA | Tryptamine | [11] |
| 5-Chloro-αET | PAL-526 | 33.2 | >10000 | IA (RI) | SRA | α-Ethyltryptamine | [11] |
| 5-Chloro-αMT | PAL-542 | 16.2 | 3434 | 54.3 | SDRA | α-Methyltryptamine | [11][12] |
| 5-Chloro-T | PAL-441 | 19.1 | >10000 | 476 | SRA | Tryptamine | [11] |
| 5-Fluoro-αET | PAL-545 | 36.6 | 5334 | 150 | SDRA | α-Ethyltryptamine | [11] |
| 5-Fluoro-αMT | PAL-544 PAL-212 | 14–19 | 78–126 | 32–37 | SNDRA | α-Methyltryptamine | [12][11][77] |
| 5-Fluoro-T | PAL-284 | 10.1 | 464 | 82.3 | SDRA | Tryptamine | [11] |
| 5-MABB (5-MBPB) | ND | ND | ND | ND | ND | Amphetamine | [116][182] |
| (S)-5-MABB | ND | 31 | 158 | 210 | SNDRA | Amphetamine | [116][182] |
| (R)-5-MABB | ND | 49 | 850 | IA | SRA | Amphetamine | [116][182] |
| 5-MAPB | ND | 64–90 | 24 | 41–459 | SNDRA | Amphetamine | [113][183] |
| (S)-5-MAPB | ND | 67 | ND | 258 | ND | Amphetamine | [183] |
| (R)-5-MAPB | ND | 184 | ND | 1951 | ND | Amphetamine | [183] |
| 5-MeO-αMT | ND | 460 | 8900 | 1500 | SNDRA | α-Methyltryptamine | [109] |
| 5-MeO-DALT | ND | >100000 | >100000 | >100000 | IA | Tryptamine | [109] |
| 5-MeO-DET | ND | IA (RI) | IA | IA | SRI | Tryptamine | [77] |
| 5-MeO-DiPT | ND | >100000 (RI) | >100000 (RI) | >100000 | IA | Tryptamine | [109][77] |
| 5-MeO-DMT | ND | >100000 (RI) | >100000 (RI) | >100000 | IA | Tryptamine | [109][77] |
| 5-MeO-DPT | ND | IA (RI) | IA | IA (RI) | SRI | Tryptamine | [77] |
| 5-MeO-MiPT | ND | >100000 | >100000 | >100000 | IA | Tryptamine | [109][77] |
| 5-MeO-NET | ND | 284 | >10000 | >10000 | SRA | Tryptamine | [77] |
| 5-MeO-NiPT | ND | IA (RI) | IA | IA | SRI | Tryptamine | [77] |
| 5-MeO-NMT | ND | 1114 | >10000 | >10000 | SRA | Tryptamine | [77] |
| 5-MeO-T | PAL-234 | 2169 | >10000 | 11031 | SDRA | Tryptamine | [11][77] |
| 5-Methyl-T | PAL-22 | 139 | >10000 | >10000 | SRA | Tryptamine | [11] |
| 6-APB | ND | 36 | 14 | 10 | SNDRA | Amphetamine | [113] |
| 6-APBT | ND | 10.7 | 13.6 | 7.2 | SNDRA | APBT | [117] |
| 6-API (6-IT) | ND | 19.9 | 25.6 | 164.0 | SNDRA | Amphetamine | [118] |
| 6-Fluoro-T | PAL-227 | 4.4 | 1575 | 106 | SRA | Tryptamine | [11] |
| 6-MABB (6-MBPB) | ND | ND | ND | ND | ND | Amphetamine | [116][182] |
| (R)-6-MABB | ND | 172 | 227 | IA | SNRA | Amphetamine | [116][182] |
| (S)-6-MABB | ND | 54 | 77 | 41 | SNDRA | Amphetamine | [116][182] |
| 6-MAPB | ND | 33 | 14 | 20 | SNDRA | Amphetamine | [113] |
| 6-MeO-T | PAL-263 | 53.8 | 465 | 113 | SNDRA | Tryptamine | [11] |
| 6-Methyl-T | PAL-522 | 51.6 | >10000 | 353 | SDRA | Tryptamine | [11] |
| 7-APBT | ND | 36.9 | 28.5 | 16.8 | SNDRA | APBT | [117] |
| 7-Chloro-T | PAL-532 | 8.03 | 656 | 1330 | SRA | Tryptamine | [11] |
| 7-MeO-T | PAL-533 | 44.6 | 5600 | 2118 | SRA | Tryptamine | [11] |
| 7-Methyl-T | PAL-286 | 23.7 | >10000 | 3380 | SRA | Tryptamine | [11] |
| α-Ethyltryptamine (AET, αET) | PAL-125 | 23.2 | 640 | 232 | SDRA | α-Ethyltryptamine | [11] |
| (–)-α-Ethyltryptamine | PAL-640 | 54.9 | 3670 | 654 | SRA | α-Ethyltryptamine | [11] |
| (+)-α-Ethyltryptamine | PAL-647 | 34.7 | 592 | 57.6 | SDRA | α-Ethyltryptamine | [11] |
| α-Me-MC (βk-mephentermine; RAD-081) | ND | 12860 | 153 | 590 | NDRA | Cathinone | [184][185][186] |
| α-Methylisotryptamine (isoAMT) | PAL-569 | 177 | 81 | 1062 | SNRA | Isotryptamine | [12] |
| α-Methyltryptamine (αMT; AMT) | PAL-17 | 21.7–68 | 79–112 | 78.6–180 | SNDRA | α-Methyltryptamine | [109][11][187] |
| βk-NMPEA (FTS-096) | ND | >60000 | 148 | 1860 | NRA | Phenethylamine | [184][185][186] |
| AMAPN | ND | 21 | ND | 55 | ND | Cathinone | [137][188] |
| Amfepramone (diethylpropion) | ND | >10000 | >10000 | >10000 | PD | Cathinone | [189][151] |
| Aminorex | ND | 193–414 | 15.1–26.4 | 9.1–49.4 | SNDRA | Phenyloxazolamine | [88][174][4][153][151] |
| Amphetamine (A) | ND | ND | ND | ND | NDRA | Amphetamine | ND |
| Dextroamphetamine | ND | 698–1765 | 6.6–10.2 | 5.8–24.8 | NDRA | Amphetamine | [88][190][4][179][151] |
| Levoamphetamine | ND | ND | 9.5 | 27.7 | NDRA | Amphetamine | [123][4][191][192] |
| APPEA (α-Pr-PEA) | PAL-550 | IA | ND | IA (RI) | ND | Amphetamine | [5][152] |
| BDB | ND | 180 | 540 | 2,300 | NDRA | Amphetamine | [109] |
| Benzylpiperazine (BZP) | ND | 6050–>10000 | 62–68 | 175–600 | NDRA | Benzylpiperazine | [109][193][3][4][194] |
| BK-NM-AMT | ND | 41.3 | ND (55% at 10 μM) | 92.8 | SDRA | α-Methyltryptamine | [137][188][138] |
| BK-5F-NM-AMT | ND | 190 | ND | 620 | ND | α-Methyltryptamine | [195] |
| BK-5Cl-NM-AMT | ND | 200 | ND | 865 | ND | α-Methyltryptamine | [195] |
| BK-5Br-NM-AMT | ND | 295 | ND | 2100 | ND | α-Methyltryptamine | [195] |
| BMAPN | ND | 27 | ND (94% at 10 μM) | 34 | SNDRA | Cathinone | [137][188] |
| BMPEA (β-Me-PEA) | ND | ND | 126 | 627 | ND | Phenethylamine | [196] |
| Bretisilocin (5F-MET; GM-2505) | ND | 8.4–15.7 (Emax = 67–71%) | ND | ND | ND | Tryptamine | [197][78] |
| Bufotenin (DMS, 5-HO-DMT) | ND | 30.5 | >10000 | >10000 | SRA | Tryptamine | [77] |
| Buphedrone (βk-MEPEA) | PAL-429 | IA | ND | 411 | ND | Cathinone | [152] |
| Bupropion (amfebutamone) | ND | IA (RI) | IA (RI) | IA (RI) | NDRI | Cathinone | [186][163][161] |
| Butylamphetamine (NBA, BA) | PAL-90 | ND | ND | IA | ND | Amphetamine | [5] |
| Butylone (βk-MBDB) | ND | 330 | IA (RI) | IA (RI) | SRA/NDRI | Cathinone | [198][199] |
| Cathinone (C; βk-AMPH) | ND | 6100–7595 | 23.6–25.6 | 34.8–83.1 | NDRA | Cathinone | [4][137][172] |
| D-Cathinone | ND | >10000 | 72.0 | 183.9 | NDRA | Cathinone | [200] |
| L-Cathinone | ND | 2366–9267 | 12.4–28 | 18–24.6 | NDRA | Cathinone | [201][163][200] |
| Chlorphentermine | ND | 18.2–30.9 | >10000 (RI) | 935–2650 | SRA | Amphetamine | [88][151] |
| DEPEA (α-Et-EPEA) | ND | ND | 209 | 604 | ND | Amphetamine | [202] |
| Dibutylone | ND | IA | IA (RI) | IA (RI) | DRI | Cathinone | [203] |
| Diethyltryptamine (DET) | ND | IA (RI) | IA | IA | SRI | Tryptamine | [77] |
| Diisopropyltryptamine (DiPT) | ND | IA (RI) | IA (RI) | IA | SRI | Tryptamine | [77] |
| Dimethylamphetamine | ND | ND | 223 | 1250 | ND | Amphetamine | [196] |
| Dimethyltryptamine (DMT) | ND | 81–114 (Emax = 81%) | 4166 | >10000 | SRA | Tryptamine | [77][78] |
| Dipropyltryptamine (DPT) | ND | >100000 (RI) | >100000 (RI) | >100000 (RI) | IA | Tryptamine | [109][77] |
| DMPP (2,3-DMPP) | PAL-218 | 24–26 (Emax = 85%) | 13.7–56 (Emax = 62%) | 1207–1320 (Emax = 66%) | SNRA | Phenylpiperazine | [76][131] |
| DMPPA (β,N,N-TMPEA) | ND | ND | 1337 (Emax = 67%) | IA | NRA | Phenethylamine | [196] |
| DOC | ND | IA | IA | IA | IA | Amphetamine | [160] |
| DOM | ND | IA | IA | IA | IA | Amphetamine | [204] |
| Dopamine (DA) | ND | >10000 (RI) | 66.2 | 86.9 | NDRA | Phenethylamine | [88][4] |
| EDMA | ND | 117 | 325 | 597 | SNDRA | Amphetamine | [110][170] |
| EDMC | ND | 347 | 327 | 496 | SNDRA | Cathinone | [110][170] |
| ENAP | PAL-1045 | 12 | 137 | 46 | SDRA | Amphetamine | [76] |
| Ephedrine (racephedrine) | ND | ND | ND | ND | NDRA | Cathinol | ND |
| D-Ephedrine (ephedrine) | ND | >10000 | 43.1–72.4 | 236–1350 | NDRA | Cathinol | [88][4] |
| L-Ephedrine | ND | >10000 | 218 | 2104 | NRA | Cathinol | [88][201] |
| Ephylone | ND | IA (RI) | IA (RI) | IA (RI) | IA (NDRI) | Cathinone | [205] |
| Epinephrine | ND | ND | ND | ND | NDRA | Phenethylamine | ND |
| Ethcathinone (EC) | ND | 1923–2118 | 88.3–99.3 | 267.6–>1000 | NRA | Cathinone | [189][4][172][179] |
| Ethylamphetamine (EA) | PAL-99 | ND | ND | 88.5 | ND | Amphetamine | [5] |
| S(+)-Ethylamphetamine | ND | 333.0 | 28.8 | 44.1 | NDRA | Amphetamine | [172][173] |
| Ethylone (βk-MDEA) | ND | 617.4 | 4251 | 1122 | SNDRA | Cathinone | [170] |
| Eutylone (βk-EBDB) | ND | 1020 | IA (RI) | IA (RI) | SRA/NDRI | Cathinone | [203] |
| Fenfluramine (3-TFM-EA) | ND | 79.3–108 | 739 | >10000 (RI) | SRA | Amphetamine | [88][206][207][4] |
| D-Fenfluramine | ND | 51.7 | 302 | >10000 | SNRA | Amphetamine | [88][206] |
| L-Fenfluramine | ND | 147 | >10000 | >10000 | SRA | Amphetamine | [206][72] |
| HHA | ND | ND | 33 | 3485 | ND | Amphetamine | [4] |
| HHMA | ND | 1729 | 77 | 130 | NDRA | Amphetamine | [4][208] |
| HHMC | ND | 14100 | 110 | 90 | NDRA | Cathinone | [209] |
| HMA | ND | 897 | 694 | 1450–3423 | SNDRA | Amphetamine | [4][210][211] |
| HMMA | ND | 589–607 | 625 | 607–3652 | SNDRA | Amphetamine | [4][210][211][208] |
| HMMC | ND | 7210 | 6340 | 5840 | SNDRA | Cathinone | [209] |
| MBDB | ND | 540 | 3300 | >100000 | SNRA | Amphetamine | [109] |
| mCPP (3-CPP, 3CPP) | ND | 28–38.1 | ≥1400 | 63000 | SRA | Phenylpiperazine | [109][72][73] |
| MDA | ND | 160–162 | 47–108 | 106–190 | SNDRA | Amphetamine | [207][4][113] |
| (R)-MDA | ND | 310 | 290 | 900 | SNDRA | Amphetamine | [207][4] |
| (S)-MDA | ND | 100 | 50.0 | 98.5 | SNDRA | Amphetamine | [207][4] |
| MDAI | ND | 114 | 117 | 1334 | SNRA | Aminoindane | [33] |
| MDC | ND | 966 | 394 | 370 | SNDRA | Cathinone | [209] |
| MDEA | PAL-192 | 47 | 2608 | 622 | SNDRA | Amphetamine | [76] |
| (R)-MDEA | PAL-193 | 52 | 651 | 507 | SNDRA | Amphetamine | [76] |
| (S)-MDEA | PAL-194 | 465 | RI | RI | SRA | Amphetamine | [76] |
| MDDMA | ND | 588.8 | IA | IA | SRA | Amphetamine | [212] |
| MDMA | ND | 50–85 | 54–110 | 51–278 | SNDRA | Amphetamine | [88][213][118][207][113] |
| (R)-MDMA | ND | 340 | 560 | 3700 | SNDRA | Amphetamine | [207][4] |
| (S)-MDMA | ND | 74 | 136 | 142 | SNDRA | Amphetamine | [207][4] |
| MDMAR | ND | ND | ND | ND | SNDRA | Phenyloxazolamine | ND |
| cis-MDMAR | ND | 43.9 | 14.8 | 10.2 | SNDRA | Phenyloxazolamine | [181] |
| trans-MDMAR | ND | 73.4 | 38.9 | 36.2 | SNDRA | Phenyloxazolamine | [181] |
| MDPV | ND | IA | 13 (Emax = 24%) | 2.3 (Emax = 24%) | NDRI | Phenylethylpyrrolidine | [190][170] |
| MDTMA | ND | IA | IA | IA | IA | Amphetamine | [212] |
| MEAI (5-MeO-AI) | ND | 134 | 861 | 2646 | SNRA | Aminoindane | [33] |
| MEPEA (α-Et-MPEA) | PAL-426 | 4698 | 58 | 179–225 | NDRA | Amphetamine | [152][202] |
| Mephedrone (4-MMC) | ND | 118.3–122 | 58–62.7 | 49.1–51 | SNDRA | Cathinone | [213][190][137][154][171] |
| S(–)-Mephedrone | ND | 61 | ND | 74 | ND | Cathinone | [179][214] |
| R(+)-Mephedrone | ND | 1470 | ND | 31 | ND | Cathinone | [179][214] |
| Mesocarb | ND | ND | ND | >100000 (RI) | DRI | Amphetamine | [215] |
| Methamphetamine (MA) | ND | ND | ND | ND | NDRA | Amphetamine | ND |
| Dextromethamphetamine | ND | 736–1292 | 12.3–14.3 | 8.5–40.4 | NDRA | Amphetamine | [88][213][4][151] |
| Levomethamphetamine | ND | 4640 | 28.5 | 416 | NRA | Amphetamine | [88][4] |
| Methcathinone (MC) | ND | 2592–5853 | 22–26.1 | 12.5–49.9 | NDRA | Cathinone | [4][137][161][154][172] |
| D-Methcathinone | ND | IA | ND | ND | NRA | Cathinone | [186] |
| L-Methcathinone | ND | 1772 | 13.1 | 14.8 | NDRA | Cathinone | [201][179] |
| Methiopropamine | ND | IA (RI) | IA (RI) | IA (RI) | NDRI | Thiopropamine | [216][217] |
| Methylone (MDMC) | ND | 234–708 | 140–270 | 117–220 | SNDRA | Cathinone | [213][190][170][203][209] |
| Methylphenidate | ND | IA (RI) | IA (RI) | IA (RI) | NDRI | Phenidate | [3][35][218] |
| Methylethyltryptamine (MET) | ND | 182.7 | ND | ND | ND | Tryptamine | [78] |
| Mexedrone (4-MMC-MeO) | ND | 2525 | IA (RI) | IA (RI) | SRA/NDRI | Cathinone | [219] |
| MiPT | ND | IA | IA | IA | IA | Tryptamine | [77] |
| MMAI | ND | 31 | 3101 | >10000 | SRA | Aminoindane | [33] |
| MNAP (methamnetamine) | PAL-1046 | 13 | 34 | 10 | SNDRA | Amphetamine | [76][5] |
| MPPA (BMMPEA, β-Me-NMPEA) | ND | ND | 154 | 574 | ND | Phenethylamine | [196] |
| Naphthylisopropylamine (NAP) | PAL-287 | 3.4 | 11.1 | 12.6 | SNDRA | Amphetamine | [220][4] |
| Naphthylmetrazine | PAL-704 | IA (RI) | 203 | 111 | NDRA/SRI | Phenylmorpholine | [157] |
| Naphthylmorpholine | PAL-678 | ND (92% at 10 μM) | ND (88% at 10 μM) | ND (79% at 10 μM) | ND | Phenylmorpholine | [157] |
| NET (NETP; N-Et-T) | PAL-536 | 18.6 | IA (RI) | IA (RI) | SRA | Tryptamine | [11][77] |
| NiPT | ND | IA (RI) | IA | IA | SRI | Tryptamine | [77] |
| NMT | PAL-152 | 22.4 | 733 | 321 | SRA | Tryptamine | [11][77] |
| Norephedrine (phenylpropanolamine) | ND | ND | ND | ND | NDRA | Cathinol | ND |
| D-Norephedrine | ND | >10000 | 42.1 | 302 | NDRA | Cathinol | [201] |
| L-Norephedrine | ND | >10000 | 137 | 1371 | NRA | Cathinol | [201] |
| Norepinephrine (NE) | ND | >10000 | 164 | 869 | NDRA | Phenethylamine | [88][4] |
| Norfenfluramine (3-TFMA) | ND | 104 | 168–170 | 1900–1925 | SNRA | Amphetamine | [206][207] |
| (+)-Norfenfluramine | ND | 59.3 | 72.7 | 924 | SNRA | Amphetamine | [206] |
| (–)-Norfenfluramine | ND | 287 | 474 | >10000 | SNRA | Amphetamine | [206] |
| Normephedrone (4-MC) | ND | 210 | 100 | 220 | SNDRA | Cathinone | [221][200][179] |
| R(+)-Normephedrone | ND | 179 | 89 | 150 | SNDRA | Cathinone | [179][200] |
| S(–)-Normephedrone | ND | 1592 | 115 | 391 | NDRA | Cathinone | [179][200] |
| Norpropylhexedrine | ND | ND | ND | ND | NDRA | Cyclohexylethylamine | ND |
| Norpseudoephedrine | ND | ND | ND | ND | NDRA | Cathinol | ND |
| D-Norpseudoephedrine (cathine) | ND | >10000 | 15.0 | 68.3 | NDRA | Cathinol | [201] |
| L-Norpseudoephedrine | ND | >10000 | 30.1 | 294 | NDRA | Cathinol | [201] |
| ODMA | ND | ND | ND | ND | SNDRA | Amphetamine | [121] |
| oMPP (2-MPP) | PAL-169 | 175 | 39.1 | 296–542 | SNDRA | Phenylpiperazine | [222][5][131] |
| PMA (4-MeO-A) | ND | ND | 166 | 867 | SNDRA | Amphetamine | [4][136][178] |
| PMMA (4-MeO-MA) | ND | ND | ND | ND | SNDRA | Amphetamine | [178] |
| (S)-PMMA | ND | 41 | 147 | 1000 | SNRA | Amphetamine | [180][223][136] |
| (R)-PMMA | ND | 134 | >14000 | 1600 | SRA | Amphetamine | [180][223][136] |
| Pentylone | ND | 476–1030 (Emax ≈ 50%) | IA (RI) | IA (RI) | SRA/NDRI | Cathinone | [198][203][205] |
| Phenacylamine (βk-PEA) | PAL-27 | >10000 | ND (96% at 10 μM) | 208 | NDRA | Phenethylamine | [5][137][179] |
| Phendimetrazine | ND | >100000 | >10000 | >10000 | PD | Phenylmorpholine | [224][4][151] |
| Phenethylamine (PEA) | ND | >10000 | 10.9 | 39.5 | NDRA | Phenethylamine | [5][123][4] |
| Phenmetrazine (PM) | PAL-55 | 7765–>10000 | 29–50.4 | 70–131 | NDRA | Phenylmorpholine | [224][4][156][157] |
| (+)-Phenmetrazine | ND | 3246 | 37.5 | 87.4 | NDRA | Phenylmorpholine | [224] |
| (–)-Phenmetrazine | ND | >10000 | 62.9 | 415 | NDRA | Phenylmorpholine | [224] |
| Phentermine (P, PH) | ND | 2575–3511 | 28.8–39.4 | 262 | NDRA | Amphetamine | [88][4][151] |
| Phenylalaninol | ND | ND | ND | ND | ND | Amphetamine | ND |
| D-Phenylalaninol | PAL-329 | >10000 | 106 | 1355 | NRA | Amphetamine | [222] |
| Phenylbutenamine | ND | ND | ND | ND | ND | Phenylbutenamine | ND |
| (3E)-Phenylbutenamine | PAL-881 | >10000 | 308 | 666 | NDRA | Phenylbutenamine | [127][128] |
| (3Z)-Phenylbutenamine | PAL-893 | >10000 | 301 | 1114 | NDRA | Phenylbutenamine | [127][128] |
| Phenylbutynamine | PAL-874 | >10000 | 305 | 688 | NDRA | Phenylbutynamine | [76] |
| Phenylisobutylamine (α-Et-PEA, AEPEA) | ND | 4698 | 80 | 225–273 | NDRA | Amphetamine | [5][152][162][202] |
| Phenylpropylamine | ND | ND | 222 | 1491 | NDRA | Phenylpropylamine | [123][4] |
| pMeOPP (4-MeOPP) | ND | 3200 | 440–1500 | 6300–11000 | SNRA | Phenylpiperazine | [109][131] |
| pMPP (4-MPP) | PAL-233 | 220 | >10000 | >20000 | SRA | Phenylpiperazine | [131][5] |
| pNPP (4-NPP) | PAL-175 | 19–43 (Emax = 57%) | >10000 | >10000 | SRA | Phenylpiperazine | [76][131] |
| Propylamphetamine (PA) | PAL-424 | ND | ND | RI (1013) | ND | Amphetamine | [5] |
| Propylcathinone (PC) | PAL-359 | ND | ND | IA | ND | Cathinone | [5][179] |
| Propylhexedrine | ND | ND | ND | ND | NDRA | Cyclohexylethylamine | ND |
| Propylone | ND | 3128 | IA (RI) | 975.9 | SDRA | Cathinone | [170] |
| Pseudoephedrine (racemic) | ND | ND | ND | ND | NDRA | Cathinol | ND |
| D-Pseudoephedrine | ND | >10000 | 4092 | 9125 | NDRA | Cathinol | [201] |
| L-Pseudoephedrine (pseudoephedrine) | ND | >10000 | 224 | 1988 | NRA | Cathinol | [201] |
| Pseudophenmetrazine | ND | >10000 | 514 | IA (RI) | NRA/DRI | Phenylmorpholine | [224] |
| (+)-Pseudophenmetrazine | ND | >10000 | 349 | 1457 | NDRA | Phenylmorpholine | [224] |
| (–)-Pseudophenmetrazine | ND | >10000 | 2511 | IA (RI) | NRA/DRI | Phenylmorpholine | [224] |
| Psilocin | PAL-153 | 561 (Emax = 54%) | >10000 | >10000 | SRA | Tryptamine | [76][77] |
| SeDMA | ND | ND | ND | ND | SNDRA | Amphetamine | [121] |
| Serotonin (5-HT) | ND | 44.4 | >10000 (RI) | ≥1960 | SRA | Tryptamine | [88][4] |
| TDMA | ND | ND | ND | ND | SNDRA | Amphetamine | [121] |
| TFMCPP (3-TFM-4-C-PP) | PAL-179 | 33 (Emax = 66%) | >10000 | >10000 | SRA | Phenylpiperazine | [76] |
| TFMPP (3-TFMPP) | ND | 121 | >10000 | >10000 | SRA | Phenylpiperazine | [193][194][4] |
| TMA (3,4,5-TMeO-A) | ND | 16000 | >100000 | >100000 | SRA | Amphetamine | [109] |
| TMA-2 (2,4,5-TMeO-A) | ND | >100000 | >100000 | >100000 | IA | Amphetamine | [109] |
| TMA-6 (2,4,6-TMeO-A) | ND | >100000 | >100000 | >100000 | IA | Amphetamine | [109] |
| Tramadol | ND | IA (RI) | IA (RI) | IA | SNRI | ND | [3] |
| Tryptamine (T) | PAL-235 | 32.6 | 716 | 164 | SDRA | Tryptamine | [77][11] |
| Tyramine | ND | 2775 | 40.6 | 119 | NDRA | Phenethylamine | [88][4] |
| Notes: (1) The smaller the value, the more potently the substance releases the neurotransmitter. (2) These values were from assays conducted using rat brain synaptosomes. Values from other methods of quantifying monoamine release, such as HEK293 cells transfected with monoamine transporters, are not fully analogous to neuronal cells and result in much different and lower potencies. As a result, they are not included in this table. | |||||||
In addition to the potencies of MRAs in terms of their MRA activity, data on the affinities (Ki) of various MRAs for the monoamine transporters (MATs) and their potencies (IC50) in acting as monoamine reuptake inhibitors (MRIs) have been published.[2][88][224][225][206][190][212][188][172][175][226][227][116][158][219][163][117][228][131][156] Activities of MRAs at the vesicular monoamine transporter 2 (VMAT2) have been published as well.[27]
Notes
[edit]- ^ MRAs that are inactive at VMAT2 include phentermine, phenmetrazine, and benzylpiperazine (BZP).[5][27] Others, including cathinones like mephedrone, methcathinone, and methylone, also show only weak VMAT2 activity (e.g., ~10-fold weaker than the corresponding amphetamines).[28][29][30]
- ^ MRAs that are inactive at the human TAAR1 include most cathinones (e.g., methcathinone, mephedrone, flephedrone, and brephedrone), ephedrine, 4-methylamphetamine (4-MA), para-methoxyamphetamine (PMA), 4-methylthioamphetamine (4-MTA), MDMA MDEA, MBDB, 5-APDB, 5-MAPDB, 4-methylaminorex derivatives, meta-chlorophenylpiperazine (mCPP), TFMPP, and methylhexanamine (DMAA), among others.[52][53][26][50][58]
References
[edit]- ^ a b c d e f g h i Heal DJ, Smith SL, Gosden J, Nutt DJ (June 2013). "Amphetamine, past and present--a pharmacological and clinical perspective". Journal of Psychopharmacology. 27 (6): 479–496. doi:10.1177/0269881113482532. PMC 3666194. PMID 23539642.
Although the pharmacological effect of amphetamine is predominantly mediated by monoamine release, this mechanism is complemented by reuptake inhibition [...] that combine additively or synergistically to augment synaptic monoamine concentrations. The description of amphetamine as a 'monoamine reuptake inhibitor' often causes some confusion, and the difference between the mechanisms of amphetamine, which is a competitive reuptake transport substrate, and classical reuptake inhibitors is illustrated in Figure 3. [...] d-Amphetamine is generally accepted to be a weak dopamine reuptake inhibitor with a Ki value of ~100 nM, a moderately potent inhibitor of noradrenaline reuptake (Ki = 40–50 nM) and a very weak inhibitor of 5-HT reuptake (Ki = 1.4-3.8 µM). [...] the efficacy of amphetamine relative to other indirect monoamine agonists, for example classical reuptake inhibitors, can only be estimated from in vivo experiments. [...] [d- and l-Amphetamine] dose-dependently increased the extracellular concentrations of noradrenaline in the prefrontal cortex (PFC) and dopamine in the striatum. The pharmacodynamics of their effects are typical of those reported for monoamine releasing agents, i.e. a fast onset of action with peak increases of noradrenaline and dopamine efflux occurring at 30–45 min, large effects (400–450% of baseline for noradrenaline and 700–1500% of baseline for dopamine), with a relatively rapid decline after the maximum (Figure 4). [...] the magnitude of the increases produced by amphetamine's isomers are greater than those reported for classical reuptake inhibitors such as atomoxetine or bupropion, and there is no dose-effect ceiling to amphetamine's actions [...] The primary action of amphetamine is to increase synaptic concentrations of monoamine neurotransmitters, thereby indirectly enhancing noradrenergic, dopaminergic neurotransmission in the CNS.
- ^ a b c d e f g h i j k l m Rothman RB, Baumann MH (October 2003). "Monoamine transporters and psychostimulant drugs". European Journal of Pharmacology. 479 (1–3): 23–40. doi:10.1016/j.ejphar.2003.08.054. PMID 14612135.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y Rothman RB, Baumann MH (2006). "Therapeutic potential of monoamine transporter substrates". Current Topics in Medicinal Chemistry. 6 (17): 1845–1859. doi:10.2174/156802606778249766. PMID 17017961.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd Blough B (July 2008). "Dopamine-releasing agents" (PDF). In Trudell ML, Izenwasser S (eds.). Dopamine Transporters: Chemistry, Biology and Pharmacology. Hoboken [NJ]: Wiley. pp. 305–320. ISBN 978-0-470-11790-3. OCLC 181862653. OL 18589888W.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as Reith ME, Blough BE, Hong WC, Jones KT, Schmitt KC, Baumann MH, et al. (February 2015). "Behavioral, biological, and chemical perspectives on atypical agents targeting the dopamine transporter". Drug and Alcohol Dependence. 147: 1–19. doi:10.1016/j.drugalcdep.2014.12.005. PMC 4297708. PMID 25548026.
Converging lines of evidence have solidified the notion that DA releasers are substrates of the transporter and once translocated, they reverse the normal direction of transporter flux to evoke release of endogenous neurotransmitters. The nature of this reversal is not well understood, but the entire process is primarily transporter-dependent and requires elevated intracellular sodium concentrations, phosphorylation of DAT, and possible involvement of transporter oligomers (Khoshbouei et al., 2003, 2004; Sitte and Freissmuth, 2010). [...] A library of approximately 1400 phenethylamine compounds (PAL compounds) has been screened using these protocols. Among the active compounds,the smaller DAT ligands were found to be DA releasers while the sterically larger compounds were DAT uptake inhibitors. [...] Generic pharmacophore for biogenic amine transporter ligands. Note that transportable substrate ligands exhibit size constraints defined by the red circle. Functional groups attached to the nitrogen, α-carbon or phenyl ring that extend beyond the "edge" of the pharmacophore will generate partial substrates, transporter blockers or be inactive. [...] phenmetrazine was found to be completely inactive at VMAT2 indicating that a direct interaction of the releaser with VMAT2 is not required for inducing neurotransmitter efflux into the extracellular space (Partilla et al., 2006). Phentermine and benzylpiperazine were also found in the same study to lack VMAT2 activity (Table 5).
- ^ a b c d e f g h Schmitt KC, Rothman RB, Reith ME (July 2013). "Nonclassical pharmacology of the dopamine transporter: atypical inhibitors, allosteric modulators, and partial substrates". The Journal of Pharmacology and Experimental Therapeutics. 346 (1): 2–10. doi:10.1124/jpet.111.191056. PMC 3684841. PMID 23568856.
- ^ a b c d e f Heal DJ, Gosden J, Smith SL (December 2014). "Dopamine reuptake transporter (DAT) "inverse agonism"--a novel hypothesis to explain the enigmatic pharmacology of cocaine". Neuropharmacology. 87: 19–40. doi:10.1016/j.neuropharm.2014.06.012. PMID 24953830.
- ^ a b c d e Shimazu S, Miklya I (May 2004). "Pharmacological studies with endogenous enhancer substances: beta-phenylethylamine, tryptamine, and their synthetic derivatives". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 28 (3): 421–427. doi:10.1016/j.pnpbp.2003.11.016. PMID 15093948. S2CID 37564231.
- ^ a b c d e Knoll J (August 2003). "Enhancer regulation/endogenous and synthetic enhancer compounds: a neurochemical concept of the innate and acquired drives". Neurochemical Research. 28 (8): 1275–1297. doi:10.1023/a:1024224311289. PMID 12834268.
- ^ Rothman RB, Blough BE, Baumann MH (January 2007). "Dual dopamine/serotonin releasers as potential medications for stimulant and alcohol addictions". The AAPS Journal. 9 (1): E1-10. doi:10.1208/aapsj0901001. PMC 2751297. PMID 17408232.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae Blough BE, Landavazo A, Partilla JS, Decker AM, Page KM, Baumann MH, et al. (October 2014). "Alpha-ethyltryptamines as dual dopamine-serotonin releasers". Bioorganic & Medicinal Chemistry Letters. 24 (19): 4754–4758. doi:10.1016/j.bmcl.2014.07.062. PMC 4211607. PMID 25193229.
- ^ a b c d e f g Banks ML, Bauer CT, Blough BE, Rothman RB, Partilla JS, Baumann MH, et al. (June 2014). "Abuse-related effects of dual dopamine/serotonin releasers with varying potency to release norepinephrine in male rats and rhesus monkeys". Experimental and Clinical Psychopharmacology. 22 (3): 274–284. doi:10.1037/a0036595. PMC 4067459. PMID 24796848.
- ^ Brust JC (2004). Neurological Aspects of Substance Abuse. Butterworth-Heinemann. pp. 117–. ISBN 978-0-7506-7313-6.
- ^ Competitive problems in the drug industry: hearings before Subcommittee on Monopoly and Anticompetitive Activities of the Select Committee on Small Business, United States Senate, Ninetieth Congress, first session. U.S. Government Printing Office. 1976. pp. 2–.
- ^ Parrott AC, Stuart M (1 September 1997). "Ecstasy (MDMA), amphetamine, and LSD: comparative mood profiles in recreational polydrug users". Human Psychopharmacology: Clinical and Experimental. 12 (5): 501–504. CiteSeerX 10.1.1.515.2896. doi:10.1002/(sici)1099-1077(199709/10)12:5<501::aid-hup913>3.3.co;2-m. ISSN 1099-1077.
- ^ Scorza C, Silveira R, Nichols DE, Reyes-Parada M (July 1999). "Effects of 5-HT-releasing agents on the extracellullar hippocampal 5-HT of rats. Implications for the development of novel antidepressants with a short onset of action". Neuropharmacology. 38 (7): 1055–1061. doi:10.1016/s0028-3908(99)00023-4. PMID 10428424.
- ^ Morean ME, de Wit H, King AC, Sofuoglu M, Rueger SY, O'Malley SS (May 2013). "The drug effects questionnaire: psychometric support across three drug types". Psychopharmacology. 227 (1): 177–192. doi:10.1007/s00213-012-2954-z. PMC 3624068. PMID 23271193.
- ^ Nelson RA, Boyd SJ, Ziegelstein RC, Herning R, Cadet JL, Henningfield JE, et al. (March 2006). "Effect of rate of administration on subjective and physiological effects of intravenous cocaine in humans". Drug and Alcohol Dependence. 82 (1): 19–24. doi:10.1016/j.drugalcdep.2005.08.004. PMID 16144747.
- ^ Berlin I, Warot D, Aymard G, Acquaviva E, Legrand M, Labarthe B, et al. (September 2001). "Pharmacodynamics and pharmacokinetics of single nasal (5 mg and 10 mg) and oral (50 mg) doses of ephedrine in healthy subjects". European Journal of Clinical Pharmacology. 57 (6–7): 447–455. doi:10.1007/s002280100317. PMID 11699608. S2CID 12410591.
- ^ Powers ME (October 2001). "Ephedra and its application to sport performance: another concern for the athletic trainer?". Journal of Athletic Training. 36 (4): 420–424. PMC 155439. PMID 16558668.
- ^ Meeusen R, Watson P, Hasegawa H, Roelands B, Piacentini MF (1 January 2006). "Central fatigue: the serotonin hypothesis and beyond". Sports Medicine. 36 (10): 881–909. doi:10.2165/00007256-200636100-00006. PMID 17004850. S2CID 5178189.
- ^ Roelands B, Meeusen R (March 2010). "Alterations in central fatigue by pharmacological manipulations of neurotransmitters in normal and high ambient temperature". Sports Medicine. 40 (3): 229–246. doi:10.2165/11533670-000000000-00000. PMID 20199121. S2CID 25717280.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x Reith ME, Gnegy ME (2020). "Molecular Mechanisms of Amphetamines". Handb Exp Pharmacol. Handbook of Experimental Pharmacology. 258: 265–297. doi:10.1007/164_2019_251. ISBN 978-3-030-33678-3. PMID 31286212.
Despite the knowledge that amphetamine is a substrate for the DAT and NET, questions still remain as to the physiological mechanism of amphetamine action. [...] At lower doses, amphetamine preferentially releases a newly synthesized pool of DA. [...] DA stores will not be depleted by the AMPT in these short time frames, leading to the conclusion that newly synthesized DA is a principal substrate for amphetamine-stimulated DA efflux. [...] Controversy has surrounded the role of VMAT2 and synaptic vesicles in the mechanism of amphetamine action. [...] Undoubtedly vesicles contribute strongly to the maximal DA released by amphetamine, although VMAT2 is not absolutely required for amphetamine to release DA from nerve terminals (Pifl et al. 1995; Fon et al. 1997; Wang et al. 1997; Patel et al. 2003). [...] Recently, a new model of amphetamine action has been formulated that proposes that amphetamine elevates tonic DA (non-exocytotic) signaling through reverse transport and depleting vesicular stores, but activates phasic DA signaling by enhancing vesicular DA release from the readily releasable pool (Covey et al. 2013). These conclusions were drawn from experiments using fast-scan cyclic voltammetry in either freely moving or anesthetized rats (Avelar et al. 2013; Daberkow et al. 2013). Again, one must strongly consider the dose of amphetamine in interpretation of these actions (Calipari and Ferris 2013).
- ^ a b c d e f g h i j Sulzer D, Sonders MS, Poulsen NW, Galli A (April 2005). "Mechanisms of neurotransmitter release by amphetamines: a review". Prog Neurobiol. 75 (6): 406–433. doi:10.1016/j.pneurobio.2005.04.003. PMID 15955613.
While the sine qua non property of AMPH at monoamine transporters is the promotion of monoamine release via reverse transport, there are yet profound mysteries in understanding how this works. It is additionally clear that AMPH is an uptake blocker as well as a releaser, and differentiating between elevating extracellular monoamines by reverse transport or uptake blockade can be difficult. Of course, the many AMPH derivatives and different transporters maintain different combinatorial properties, an important topic beyond the range of this article. [...] The mechanism of how reverse transport occurs is unknown, and a very old issue of how reserpine can inhibit uptake but not halt reverse transport remains opaque.
- ^ a b c d Sitte HH, Freissmuth M (January 2015). "Amphetamines, new psychoactive drugs and the monoamine transporter cycle". Trends Pharmacol Sci. 36 (1): 41–50. doi:10.1016/j.tips.2014.11.006. PMC 4502921. PMID 25542076.
[...] most amphetamines are [monoamine transporter] substrates, which pervert the relay to elicit efflux of monoamines into the synaptic cleft. However, some amphetamines act as transporter inhibitors. [...] Amphetamines also bind to the trace amine receptors TAR1, [...] TAR1 is not activated by all psychoactive amphetamines (p-chloroamphetamine, for instance, is inactive); stimulation of TAR1 actually reduces dopamine release and thus decreases sensitivity to amphetamine [18,19]. [...] amphetamines are taken up by plasma-membrane monoamine transporters as exogenous substrates [31]. Accordingly, they inhibit the physiological monoamine reuptake in a competitive manner [36]. As a consequence of both amphetamine-induced reverse transport and inhibition of reuptake, the synaptic monoamine concentration increases, which in turn activates post- and presynaptic receptors [37]. The activation of postsynaptic receptors propagates the signal and contributes to the biological response. Stimulation of presynaptic autoreceptors decreases the quantal release of monoamines upon excitatory inputs; [...]
- ^ a b c d e Kuropka P, Zawadzki M, Szpot P (May 2023). "A narrative review of the neuropharmacology of synthetic cathinones-Popular alternatives to classical drugs of abuse". Hum Psychopharmacol. 38 (3): e2866. doi:10.1002/hup.2866. PMID 36866677.
An interesting neurochemical issue is the interaction between compounds acting as blockers and substrates. [...] Substrates (e.g. mephedrone) use MAT proteins to release neurotransmitters, while inhibitors (e.g. [MDPV]) prevent the transport of any compounds through MATs. It follows that simultaneous use of a substrate and a blocker should result in an antagonistic mechanism that lowers the mutual potency. Paradoxically, MDPV and mephedrone occur together in mixtures, and in addition they reinforce each other's effects, resulting in very strong stimulation. Simultaneous use of both SCs is reported by users, and studies in rodents involving simultaneous administration of the drugs have shown a significant increase in locomotor activity and additive effect compared to administering these drugs alone (Allen et al., 2019; Benturquia et al., 2019). [...] The explanation for this phenomenon can be found in the action of organic cation transporter (OCT) proteins. OCTs are a family of proteins responsible for endothelial transport of small, organic, hydrophilic, and positively charged molecules, including neurotransmitters and xenobiotics (Couroussé & Gautron, 2015). OCT3 is a protein present in the dopaminergic regions of the central nervous system, where it promotes DA reuptake when it is inhibited for high affinity transporters (DAT) (Couroussé & Gautron, 2015). Monoamines can also be released by OCTs. [...] Ex vivo studies on superior cervical ganglia cells enriched in NET and OCT3 showed that in the presence of MDPV blocking MAT proteins, mephedrone causes neurotransmitter efflux through OCT3, which is insensitive to the inhibitory effects of MDPV. The release of monoamines through OCT3, a low‐affinity transporter, presumably explains the paradoxical synergistic effects of inhibitors and substrates (Mayer et al., 2019). [...] Another feature that distinguishes [synthetic cathinones (SCs)] from amphetamines is their negligible interaction with the trace amine associated receptor 1 (TAAR1). Activation of this receptor reduces the activity of dopaminergic neurones, thereby reducing psychostimulatory effects and addictive potential (Miller, 2011; Simmler et al., 2016). Amphetamines are potent agonists of this receptor, making them likely to self‐inhibit their stimulating effects. In contrast, SCs show negligible activity towards TAAR1 (Kolaczynska et al., 2021; Rickli et al., 2015; Simmler et al., 2014, 2016). [...] It is worth noting, however, that for TAAR1 there is considerable species variability in its interaction with ligands, and it is possible that the in vitro activity of [rodent TAAR1 agonists] may not translate into activity in the human body (Simmler et al., 2016). The lack of self‐regulation by TAAR1 may partly explain the higher addictive potential of SCs compared to amphetamines (Miller, 2011; Simmler et al., 2013).
- ^ a b c Partilla JS, Dempsey AG, Nagpal AS, Blough BE, Baumann MH, Rothman RB (October 2006). "Interaction of amphetamines and related compounds at the vesicular monoamine transporter". J Pharmacol Exp Ther. 319 (1): 237–246. doi:10.1124/jpet.106.103622. PMID 16835371.
A number of test drugs displayed no activity in the [3H]dopamine uptake inhibition assay (Table 1). For example, (+)- phenmetrazine and (–)-phenmetrazine, the major metabolites of phendimetrazine (Rothman et al., 2002), were essentially inactive. [...] In contrast, other amphetamine-type agents, such as phentermine, phenmetrazine, and 1-benzylpiperazine, are potent releasers of neuronal dopamine (Baumann et al., 2000, 2005; Rothman et al., 2002), but they are inactive at VMAT2. Agents such as these may prove to be valuable control compounds for determining the importance of vesicular release for the in vivo actions of amphetamine-type agents.
- ^ a b c d Oeri HE (May 2021). "Beyond ecstasy: Alternative entactogens to 3,4-methylenedioxymethamphetamine with potential applications in psychotherapy". J Psychopharmacol. 35 (5): 512–536. doi:10.1177/0269881120920420. PMC 8155739. PMID 32909493.
- ^ a b Pifl C, Reither H, Hornykiewicz O (May 2015). "The profile of mephedrone on human monoamine transporters differs from 3,4-methylenedioxymethamphetamine primarily by lower potency at the vesicular monoamine transporter". Eur J Pharmacol. 755: 119–126. doi:10.1016/j.ejphar.2015.03.004. PMID 25771452.
- ^ Cozzi NV, Sievert MK, Shulgin AT, Jacob P, Ruoho AE (September 1999). "Inhibition of plasma membrane monoamine transporters by beta-ketoamphetamines". Eur J Pharmacol. 381 (1): 63–69. doi:10.1016/s0014-2999(99)00538-5. PMID 10528135.
- ^ Wimalasena K (July 2011). "Vesicular monoamine transporters: structure-function, pharmacology, and medicinal chemistry". Med Res Rev. 31 (4): 483–519. doi:10.1002/med.20187. PMC 3019297. PMID 20135628.
- ^ Simmler LD (2018). "Monoamine Transporter and Receptor Interaction Profiles of Synthetic Cathinones". Synthetic Cathinones. Current Topics in Neurotoxicity. Vol. 12. Cham: Springer International Publishing. pp. 97–115. doi:10.1007/978-3-319-78707-7_6. ISBN 978-3-319-78706-0.
While the determination of drug effects at the isolated target (i.e., DAT, NET, and SERT) can characterize the direct drug action at the target protein, other physiological components can also contribute significantly to the overall effect of the drug. It has been proposed that transporter-mediated, drug-induced efflux of neurotransmitter occurs through effects on the vesicular monoamine transporter 2 (VMAT2), depleting neurotransmitter from the vesicles into the cytosol (Nickell et al. 2014). Accordingly, full assessment of release would require testing the effects of a drug on the membrane transporters (SERT, DAT, and NET) and the effects of a drug at VMAT2. Alternatively, a more physiological system, such as synaptosomes or brain slices, could be used. However, reverse transport can also occur in cell lines that only express the plasma membrane transporters but not VMAT2 (Eshleman et al. 2013; Scholze et al. 2000) and in synaptosomes when VMAT2 is inhibited (Rothman et al. 2001).
- ^ a b c d e f g Halberstadt AL, Brandt SD, Walther D, Baumann MH (March 2019). "2-Aminoindan and its ring-substituted derivatives interact with plasma membrane monoamine transporters and α2-adrenergic receptors". Psychopharmacology (Berl). 236 (3): 989–999. doi:10.1007/s00213-019-05207-1. PMC 6848746. PMID 30904940.
In contrast to assay systems involving non-neuronal cells transfected with transporter proteins, synaptosomes possess all of the cellular machinery necessary for neurotransmitter synthesis, release, metabolism, and reuptake. Synaptosomes, however, do not model all of the effects of amphetamine-type agents because the use of reserpine removes any contribution of the vesicular monoamine transporter VMAT2 (SLC18A2) to the release process. In addition to acting as a substrate for plasma membrane monoamine transporters, amphetamine also binds to VMAT, resulting in the redistribution of monoamines from vesicular stores to the cytoplasm (Sulzer et al. 1995; Partilla et al. 2006; Freyberg et al. 2016). Although transporter substrates can induce monoamine release in the absence of VMAT binding (Fon et al. 1997), it is important to recognize that 2-aminoindans may have effects in intact nerve terminals that are not fully replicated in synaptosomes. Follow-up studies will be conducted to evaluate whether 2-aminoindans are capable of interacting with VMAT.
- ^ a b c Sulzer D, Cragg SJ, Rice ME (August 2016). "Striatal dopamine neurotransmission: regulation of release and uptake". Basal Ganglia. 6 (3): 123–148. doi:10.1016/j.baga.2016.02.001. PMC 4850498. PMID 27141430.
2.2.1. DAT regulation by psychostimulants [...] Considerable evidence supports a role for DAT substrates, like amphetamine, in inducing DAT internalization in vivo and in vitro, thus decreasing DA uptake [390–395]. [...] While several kinases are involved in the regulation of DAT, PKC is by far the most thoroughly investigated [388,403]. PKC activation induces DAT internalization [393,404–406] although the mechanism of PKC activation by DAT substrates remains largely unknown [388,389,403,407,408]
- ^ a b c d e f g Docherty JR, Alsufyani HA (August 2021). "Pharmacology of Drugs Used as Stimulants". J Clin Pharmacol. 61 Suppl 2: S53 – S69. doi:10.1002/jcph.1918. PMID 34396557.
Release by an indirect agonist is termed reverse transport and may require buildup of neurotransmitter in the nerve cytoplasm [...] Stimulants can act to stimulate presynaptic (CNS) or prejunctional (periphery) receptors for the neurotransmitter on nerve terminals to control release from those endings. These receptors are usually inhibitory and are marked as I (either NE, DA, or 5-HT inhibitory receptor) in Figure 1 and as α2 (inhibitory α2- adrenoceptor) in Figure 2, respectively. For instance, α2-adrenoceptors are present as autoreceptors on noradrenergic nerves and mediate an inhibition of NE release both in the periphery and CNS (see Figures 1 and 2).71 [...] Stimulants can act to stimulate, either directly or indirectly via increased release of the monoamine neurotransmitter, receptors for the neurotransmitter on nerves or effector cells situated postsynaptically/postjunctionally to the monoaminergic neuron. [...] Receptor-mediated actions of amphetamine and other amphetamine derivatives [...] may involve trace amine-associated receptors (TAARs) at which amphetamine and MDMA also have significant potency.85–87 Many stimulants have potency at the rat TAAR1 in the micromolar range but tend to be about 5 to 10 times less potent at the human TAAR1, [...] Activation of the TAAR1 receptor causes inhibition of dopaminergic transmission in the mesocorticolimbic system, and TAAR1 agonists attenuated psychostimulant abuse-related behaviors.89 It is likely that TAARs contribute to the actions of specific stimulants to modulate dopaminergic, serotonergic, and glutamate signaling,90 and drugs acting on the TAAR1 may have therapeutic potential.91 In the periphery, stimulants such as MDMA and cathinone produce vasoconstriction, part of which may involve TAARs, although only relatively high concentrations produced vascular contractions resistant to a cocktail of monoamine antagonist drugs.86
- ^ a b c d e Vaughan RA, Henry LK, Foster JD, Brown CR (2024). "Post-translational mechanisms in psychostimulant-induced neurotransmitter efflux". Advances in Pharmacology. Vol. 99. Elsevier. pp. 1–33. doi:10.1016/bs.apha.2023.10.003. ISBN 978-0-443-21933-7. ISSN 1054-3589. PMID 38467478.
The characteristics and mechanisms of efflux are complex and incompletely understood, and have been summarized in many comprehensive reviews including (Reith & Gnegy, 2020; Robertson, Matthies, & Galli, 2009; Sitte & Freissmuth, 2015). [...] Early studies implicating protein phosphorylation in AMPH-evoked DA efflux were performed by Giambalvo, who demonstrated that DAT-mediated uptake of AMPH impacted the activity and subcellular localization of protein kinase C (PKC) with characteristics that correlated with DA efflux (Giambalvo, 1992), and Gnegy and colleagues, whose many studies reinforced the relationship between efflux, kinases, and ionic conditions including PKC, PKCβ, Ca2+, and Ca1+-calmodulin regulated protein kinase (CaMK) (Gnegy et al., 2004; Johnson, Guptaroy, Lund, Shamban, & Gnegy, 2005; Kantor, Hewlett, & Gnegy, 1999). [...] With respect to DAT most studies have focused on PKC, CaMK, and mitogen activated protein kinases (MAPKs), but many other signaling and kinase pathways have been implicated in efflux mechanisms for all of the MATs (Bermingham & Blakely, 2016; Vaughan & Foster, 2013). [...] DAT phosphorylation stimulated by AMPH or METH also occurs on this domain and is blocked by PKC inhibitors (Cervinski et al., 2005; Karam et al., 2017), indicating the capacity of the drugs to involve the PKC pathway. How this occurs is not known, but could potentially follow from drug perturbation of local ion/Ca2+ concentrations that impact PTM enzymes, or alternatively could occur by substrate-driven induction of transporter conformations in which phosphorylation sites become more or less available to enzyme action. [...] There are many other Ser and Thr residues on DAT intracellular loops and domains that may serve as phosphorylation sites, and in vitro studies have demon- strated phosphorylation of N— and C—terminal peptide sequences by many kinases in addition to PKC, ERK, and CaMK that have been implicated in regulation and efflux including protein kinase A (PKA), protein kinase G (PKG), casein kinase 2 (CK2), p38 kinase, JNK2, Cdk5, and Akt1 (Gorentla I et al., 2009; Vaughan & Foster, 2013). [...] The regulatory, efflux, and post-translational characteristics of NET and SERT show many similarities to DAT that indicate conservation of mechanism, but also some distinct properties that reflect requirements of specific neuronal populations. [...] With respect to efflux there are many similarities between SERT, NET, and DAT that indicate conservation of mechanisms.
- ^ a b c Schmitt KC, Reith ME (February 2010). "Regulation of the dopamine transporter: aspects relevant to psychostimulant drugs of abuse". Ann N Y Acad Sci. 1187: 316–340. doi:10.1111/j.1749-6632.2009.05148.x. PMID 20201860.
However, another significant question remains: how might amphetaminergic substrates activate PKC in the first place? PKC activity is regulated by Ca2+ and diacylglycerol, a phospholipid metabolite generated in concert with inositol triphosphate by the enzyme phospholipase C (PLC), which is also Ca2+ dependent. [...] Usually, PLC is activated by agonist binding at GPCRs coupled to the Gq/11- type α-subunit; however, compounds, such as amphetamine and methamphetamine, lack significant affinity for GPCRs other than the trace amine-associated receptor 1 (TAAR1), a Gs-coupled receptor.74 [...] Interestingly, inhibition of the Na+/Ca2+ antiporter with amiloride also blocked amphetamine-induced PKC activation, suggesting that the ionic effects of DAT substrate translocation can directly influence activation of intracellular signaling cascades. When substrates are transported across the plasma membrane via the DAT, sodium ions are cotransported, and this increase in intracellular sodium concentration may cause Na+/Ca2+ antiporters at mitochondrial and endoplasmic reticulum membranes to operate in reverse, favoring a net flux of Ca2+ into the cytosolic compartment. [...]
- ^ Steinkellner T, Montgomery TR, Hofmaier T, Kudlacek O, Yang JW, Rickhag M, et al. (May 2015). "Amphetamine action at the cocaine- and antidepressant-sensitive serotonin transporter is modulated by αCaMKII". J Neurosci. 35 (21): 8258–8271. doi:10.1523/JNEUROSCI.4034-14.2015. PMC 4444546. PMID 26019340.
Amphetamine-induced transport reversal at the closely related dopamine transporter (DAT) has been shown previously to be contingent upon modulation by calmodulin kinase IIα (αCaMKII). Here, we show that not only DAT, but also SERT, is regulated by αCaMKII. Inhibition of αCaMKII activity markedly decreased amphetamine-triggered SERT-mediated substrate efflux in both cells coexpressing SERT and αCaMKII and brain tissue preparations. [...] Moreover, we found that genetic deletion of αCaMKII impaired the locomotor response of mice to [MDMA] and blunted d-fenfluramine-induced prolactin release, substantiating the importance of αCaMKII modulation for amphetamine action at SERT in vivo as well. SERT-mediated substrate uptake was neither affected by inhibition of nor genetic deficiency in αCaMKII.
- ^ Bermingham DP, Blakely RD (October 2016). "Kinase-dependent Regulation of Monoamine Neurotransmitter Transporters". Pharmacol Rev. 68 (4): 888–953. doi:10.1124/pr.115.012260. PMC 5050440. PMID 27591044.
- ^ Støier JF, Konomi-Pilkati A, Apuschkin M, Herborg F, Gether U (August 2023). "Amphetamine-induced reverse transport of dopamine does not require cytosolic Ca2". J Biol Chem. 299 (8): 105063. doi:10.1016/j.jbc.2023.105063. PMC 10448275. PMID 37468107.
[...] AMPH is a substrate of DAT and causes nonexocytotic efflux of DA by reversing the direction of transport via DAT through a yet not fully understood mechanism (4–7). To improve our insights into AMPH-induced efflux with a focus on the unsettled role of Ca2+, we establish here a novel approach enabling simultaneous assessment of DA efflux and intracellular signaling pathways by live fluorescent imaging of cultured DA midbrain neurons. [...] our data provide strong evidence that AMPH-induced DA efflux via DAT in DArgic neurons does not require Ca2+ but primarily relies on the concerted action of AMPH on VMAT2 and DAT. [...] [...] Summarized, we employ a live imaging approach enabling parallel monitoring of DA efflux and activation of intracellular signaling pathways in cultured DArgic neurons. Our data reveal in the neurons profound AMPH-induced DA efflux that strikingly neither requires Ca2+ signaling nor activation of the kinases PKC and CaMKIIα. However, the efflux depends on both the activity of VMAT2 and DAT, substantiating the unequivocal concerted importance of both transporters for the pharmacological action of AMPH on DArgic neurons. [...]
- ^ a b Miller GM (March 2012). "Avenues for the development of therapeutics that target trace amine associated receptor 1 (TAAR1)". J Med Chem. 55 (5): 1809–1814. doi:10.1021/jm201437t. PMC 3618978. PMID 22214431.
Although a detailed and rigorous description of the regional distribution of TAAR1 protein and mRNA expression has yet to be accomplished, it is established that TAAR1 protein and mRNA are expressed in monoaminergic brain regions.3,16,26 In our laboratory, we exploited our prowess with assessing changes in kinetic activity of the dopamine transporter (DAT), norepinephrine transporter (NET) and serotonin transporter (SERT) to assess TAAR1 functionality. Because many of the identified ligands that activate TAAR1 are also substrates at the monoamine transporters and TAAR1 localization in transfected cells was shown to remain largely intracellular,4 we had reasoned early on that monoamine transporters could serve as conduits for TAAR1 agonists to enter cells, thereby providing access of the agonist to an intracellular pool of TAAR1 receptors. We speculated that if this were the case there could be a special relationship between TAAR1 and monoamine transporters because they share some of the same ligands. Indeed, we observed substantially enhanced CRE-luciferase signaling in transfected cells that co-expressed both TAAR1 and a monoamine transporter (DAT, NET or SERT).9,16 Because monoamine transporter kinetic regulation and internalization is a consequence of upregulated cellular phosphorylation cascades,27,28,29 we reasoned that the enhanced TAAR1 signaling could in turn trigger changes in the kinetic activity of the monoamine transporters under conditions of co-localization. This too was born out in a series of studies from our laboratory which demonstrated that TAAR1 activation drives the PKA and PKC cellular signaling cascades that result in inhibition of monoamine uptake and transporter reversal (efflux) in DAT/TAAR1, NET/TAAR1 and SERT/TAAR1 co-transfected cells in vitro, as well as in mouse and primate striatal (DAT, SERT) and thalamic (NET) synaptosomes ex vivo.22,23,24,25,30 TAAR1 specificity for mediation of the observed kinetic effects on the monoamine transporters was further confirmed in these studies by demonstrating the absence of noncompetitive effects of the trace amine beta-phenylethylamine (β-PEA),23 the common biogenic amines,24 and methamphetamine25 on uptake inhibition and substrate-induced monoamine efflux in synaptosomes generated from TAAR1 knockout mice. Accordingly, specific drugs that target TAAR1 will likely result in alterations in monoamine kinetic function and brain monoamine levels via this mechanism.
- ^ a b c d e f Miller GM (January 2011). "The emerging role of trace amine-associated receptor 1 in the functional regulation of monoamine transporters and dopaminergic activity". Journal of Neurochemistr


 French
French Deutsch
Deutsch